TW: mentions of drugs, alcohol, self-harm & suicide.
You might be as shocked as I am to find out that about 78% of adults with Borderline Personality Disorder (BPD) develop some sort of addiction in their lives. It is so prevalent that among those in treatment for addictions, about 26.7% have BPD (Tomko et al, 2014). It has been found that people with BPD tend to drop out of treatment more frequently and have shorter phases of abstinence. As someone with BPD who has worked in treatment centres for addiction, I can see how important it is to acknowledge these statistics as more specialised treatment needs to be offered to these individuals.
Dual Diagnosis: BPD and Substance Dependence
Understanding how BPD and addiction often develop together can usually be traced back to the symptoms of BPD. People with BPD may turn to substances as a way to cope with overwhelming emotions or escape from a painful reality. Several key factors link BPD symptoms to a higher risk of addiction:
Self-Medicating
BPD often brings deep feelings of emptiness and extreme boredom, making substances an easy way to cope. Drugs or alcohol can numb painful emotions and provide temporary relief or excitement in an otherwise dull or overwhelming emotional landscape
Genetics
There may also be a genetic link between BPD and addiction. A genetic predisposition to BPD could increase the likelihood of developing substance use issues (Few et al, 2014).
Impulsive Behaviour
Research, such as that by Mitolo et al. (2024), shows that people with BPD can have structural changes in brain areas responsible for impulse control and emotional regulation. This lack of impulse control can lead to reckless substance use or even behavioural addictions.
Neglect & Trauma
Many people with BPD grow up in neglectful environments (Porter et al, 2020), where a lack of parental supervision can lead to early exposure to drugs and alcohol. Additionally, trauma during childhood is common in people with BPD, and substances may be used to escape or numb the pain from these traumatic experiences.
Self-Harm
Feelings of low self-worth, combined with emotional pain, can sometimes lead people with BPD to use substances as a form of self-harm or punishment. This destructive behaviour can further deepen the cycle of addiction.
By understanding how these factors intersect, we can better see why individuals with BPD are at a higher risk of developing addiction, often using substances as a way to cope with the intense emotions and challenges that come with the disorder.
Understanding Addiction
In the 18th and 19th centuries, addiction was often associated with moral degradation. People who struggled with substance use, particularly alcohol (often referred to as “drunkenness”), were labelled as irresponsible or socially deviant. There was little understanding of the physiological or psychological factors that contributed to addiction, and treatment often focused on punishment, shame, or strict religious and social reform.
It wasn’t until the 20th century that addiction began to be viewed more as a medical condition. Early medical models, however, still focused heavily on the addictive nature of substances themselves, without much understanding of the underlying psychological, social, or environmental factors. Addicts were often blamed for their own condition, and the idea that addiction was a voluntary choice remained widespread until more comprehensive theories of addiction emerged in the late 20th century.
One of these theories came from Bruce Alexander’s famous “Rat Park” experiment in the late 1970s. His study looked at how environments play a major role in addiction. Rats kept in isolated, barren cages with access to drug-laced water became addicted. However, when placed in “Rat Park,” a stimulating environment filled with social interaction and plenty of space to explore, the rats barely touched the drugs. This showed that addiction isn’t just about the drug itself, it’s heavily influenced by factors like living conditions, social connections, and overall well-being.
For someone with BPD, it’s easy to see how substance use could start as a way to numb emotional pain or add excitement to life. The relief substances provide, quickly lead to repeated use, which eventually turns into dependency. Having an addiction comes with a plethora of additional problems as well as exacerbating symptoms of BPD. Understanding addiction in this way highlights the importance of looking beyond just the substance and addressing the deeper issues behind it.
Why Traditional Recovery Models Fall Short for BPD
Focus on Abstinence Without Addressing Emotional Dysregulation
Many addiction recovery programs, such as 12-step models, emphasize willpower, personal accountability, and strict abstinence. While these can be effective for some, they don’t address the extreme emotional dysregulation that drives substance use in those with BPD. Without tools to manage distress, relapse is more likely.
Lack of Trauma-Informed Care
A significant number of people with BPD have a history of trauma, which fuels both addiction and emotional instability. Many traditional programs don’t integrate trauma therapy, meaning the root causes of substance use are left unaddressed.
Rigid, One-Size-Fits-All Structures
Programs like Cognitive Behavioural Therapy (CBT) are commonly used in addiction treatment, but they may not be effective for individuals with BPD, who often respond better to Dialectical Behaviour Therapy (DBT). DBT specifically helps with distress tolerance, emotional regulation, and impulsivity; key factors in both BPD and addiction recovery.
Stigma and Misunderstanding in Treatment Settings
Many addiction treatment providers are unfamiliar with BPD or hold negative biases against individuals with the disorder. This can lead to a lack of patience, misdiagnosis, or even refusal to treat patients who are seen as “too difficult.”
Difficulty with Group-Based Therapy Models
Many recovery programs rely heavily on group therapy, which can be overwhelming for someone with BPD due to intense fear of abandonment, rejection sensitivity, or difficulty managing interpersonal relationships. Without adaptations, group therapy can actually increase distress.
Why a More Nuanced, Compassionate Approach is Needed
Integration of DBT and Trauma-Informed Care
Treatment programs should incorporate DBT, which is proven to help those with BPD manage emotions and reduce impulsive behaviours, including substance use. Trauma therapy (such as EMDR or somatic therapy) is also essential for long-term healing.
Flexible and Individualized Treatment Plans
Since people with BPD often struggle with rigid structures, treatment should allow for flexibility in engagement, relapse prevention strategies, and therapeutic approaches tailored to their needs.
Compassionate, Non-Judgmental Support
A more empathetic and patient approach is needed to support individuals with BPD, recognizing that setbacks are part of their recovery process rather than signs of failure.
A Holistic Focus on Emotional Regulation and Identity Formation
Many individuals with BPD struggle with identity issues, which can make long-term sobriety difficult. Programs should include therapies that help build a stable sense of self and purpose beyond addiction.
By acknowledging these gaps and implementing more specialized, compassionate treatment approaches, we can improve outcomes for individuals with BPD struggling with addiction.
Action Plan for Someone with BPD and Substance Misuse Disorder:
If you have BPD and struggle with substance misuse, finding ways to cope with both challenges can feel overwhelming. But there are plenty of positive strategies that can help you manage both at the same time. Here are some ideas to get started:
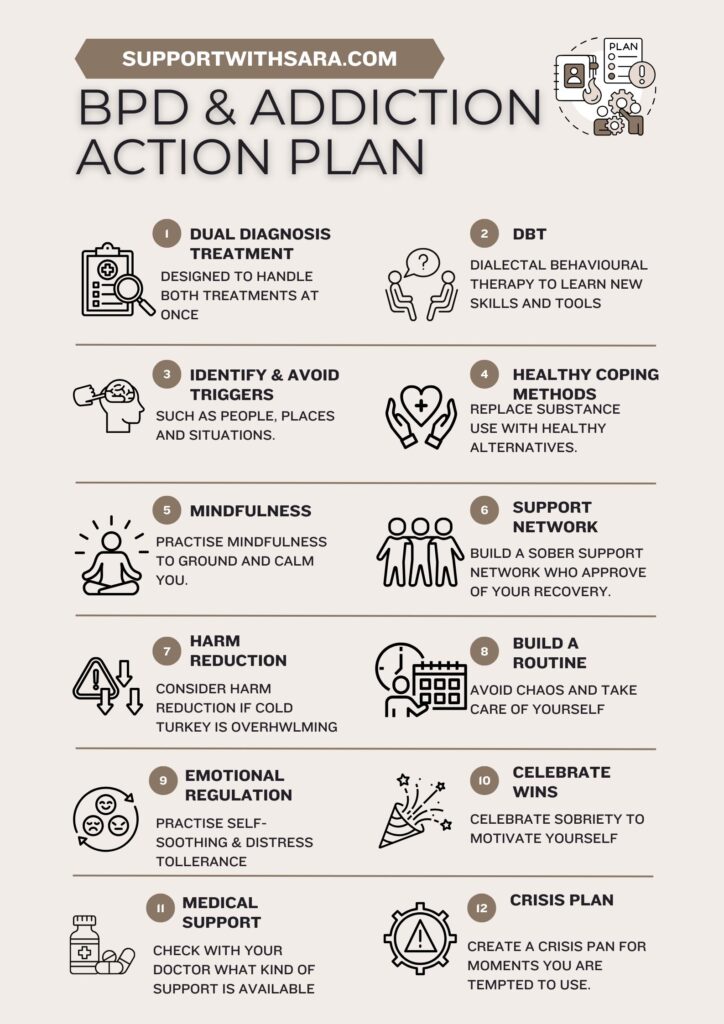
1. Look for Dual Diagnosis Treatment
- Finding a treatment program that addresses both BPD and substance misuse is key. Dual diagnosis programs are designed to handle both issues at once, offering therapy, medical support, and practical tools that increase your chances of recovery and emotional balance.
2. Try Dialectical Behavior Therapy (DBT)
- DBT is a great option if you’re dealing with both BPD and substance misuse. It teaches skills like emotional regulation, distress tolerance, mindfulness, and how to have better relationships. These tools can help you manage cravings, reduce impulsive decisions, and replace harmful habits with healthier ones.
3. Identify and Avoid Triggers
- Take note of the people, places, and situations that set off emotional distress or make you want to use. Learning to avoid or better manage these triggers can make a big difference in reducing both emotional overwhelm and the urge to use substances.
4. Find Healthy Alternatives
- Replace substance use with positive activities like exercise, journaling, or creative outlets. These activities can act as healthy distractions and also provide a way to process and channel your emotions in a constructive way.
5. Practice Mindfulness and Grounding
- Mindfulness helps you stay present in the moment, which can reduce the impulsive urge to turn to substances when you’re feeling emotionally overwhelmed. Grounding techniques like deep breathing, meditation, or focusing on your surroundings can also help you stay calm and focused.
6. Build a Sober Support Network
- Surround yourself with people who support your recovery. This could be through group therapy, 12-step meetings like AA or NA, or spending time with sober friends and family. A strong support network can make it easier to stay sober and manage BPD symptoms.
7. Consider a Harm Reduction Approach
- If the idea of quitting substances cold turkey feels too overwhelming, a harm reduction approach might be helpful. This means cutting down on use or avoiding especially dangerous behaviours, while working toward full sobriety and emotional regulation over time.
8. Stick to a Routine
- Having a daily routine can provide structure and help you avoid the chaos that often comes with substance misuse and BPD. Include self-care, meals, exercise, and therapy or sober activities in your schedule to help you stay on track.
9. Work on Emotional Regulation
- Practice skills that help you manage intense emotions, like self-soothing, delaying reactions, or using distress tolerance techniques (for example, distracting yourself or using ice to calm down). These skills can prevent you from reaching for substances to cope with emotional triggers.
10. Celebrate Small Wins
- Recovery is a journey, and it’s important to celebrate the small victories along the way. Whether it’s staying sober for a day, using a coping skill instead of turning to substances, or reaching out for help, acknowledging your progress will motivate you to keep going.
11. Consider Medication-Assisted Treatment (MAT)
- For some people, medications like Suboxone, methadone, or medications for anxiety or depression can help manage cravings and stabilise your mood. Work with a doctor who understands both BPD and substance misuse to explore these options.
12. Have a Crisis Plan
- Create a plan for those moments when you feel overwhelmed and tempted to use. This could involve calling a trusted person, using a coping skill, or going to a safe space. Having a plan in place can reduce the likelihood of turning to substances impulsively.
The Importance of Recognising BPD in Addiction Treatment
Given the high prevalence of substance use among people with Borderline Personality Disorder (BPD), it is crucial that addiction treatment programs recognize and address their unique challenges. Traditional addiction treatment approaches often fail to consider the emotional dysregulation, impulsivity, and deep-seated trauma that many individuals with BPD experience, leading to higher dropout rates and lower success in maintaining sobriety.
By integrating specialized supports (such as dual diagnosis treatment, Dialectical Behavior Therapy, trauma-informed care, and individualized harm reduction strategies) treatment centers can significantly improve outcomes for individuals with BPD. Without tailored interventions, the cycle of self-medication and addiction continues, exacerbating the emotional distress that fuels substance use in the first place.
Recognizing the connection between BPD and addiction is not just about improving treatment effectiveness, it’s about acknowledging the lived experiences of those struggling and ensuring they receive compassionate, appropriate care. A system that understands the complexities of both conditions and provides holistic, patient-centred solutions will lead to better recovery outcomes, improved mental well-being, and ultimately, saved lives.
Sources:
Childs, E., Lutz, J. A., & de Wit, H. (2017). Dose-related effects of delta-9-THC on emotional responses to acute psychosocial stress. Drug and alcohol dependence, 177, 136-144.
Few, L. R., Grant, J. D., Trull, T. J., Statham, D. J., Martin, N. G., Lynskey, M. T., & Agrawal, A. (2014). Genetic variation in personality traits explains genetic overlap between borderline personality features and substance use disorders. Addiction, 109(12), 2118-2127.
Mitolo, M., D’Adda, F., Evangelisti, S., Pellegrini, L., Gramegna, L. L., Bianchini, C., … & Tonon, C. (2024). Emotion dysregulation, impulsivity and anger rumination in borderline personality disorder: the role of amygdala and insula. European Archives of Psychiatry and Clinical Neuroscience, 274(1), 109-116.
Porter, C., Palmier‐Claus, J., Branitsky, A., Mansell, W., Warwick, H., & Varese, F. (2020). Childhood adversity and borderline personality disorder: a meta‐analysis. Acta Psychiatrica Scandinavica, 141(1), 6-20.
Scamaldo, K. M., Tull, M. T., & Gratz, K. L. (2021). Motives for opioid use explain the relation between borderline personality disorder pathology and opioid use problems. Psychiatry Research, 296, 113609.
Tomko, R. L., Trull, T. J., Wood, P. K., & Sher, K. J. (2014). Characteristics of borderline personality disorder in a community sample: comorbidity, treatment utilization, and general functioning. Journal of personality disorders, 28(5), 734-750.
United Nations Office on Drugs and Crime. (2021). World drug report 2021. https://www.unodc.org/unodc/en/data-and-analysis/wdr2021.html
World Health Organization. (2021). Opioid overdose. https://www.who.int/news-room/fact-sheets/detail/opioid-overdose