What is BPD?
BPD affects about 1-2% of the population and despite the prevalence is one of the most stigmatised mental health conditions amongst the general public (Furnham et al, 2015). It is a common experience for people with BPD to face stigma from medical professionals too; Markham and Trower (2003) found that medical professionals reported feeling less empathy and optimism and more hostility towards patients with BPD when compared to other disorders. Although it is well known in research that BPD symptoms reduce over time in individuals and recovery rates and very successful compared to most other mental health conditions, it sadly has one of the highest rates of mortality, with 10% of people with BPD dying by suicide.
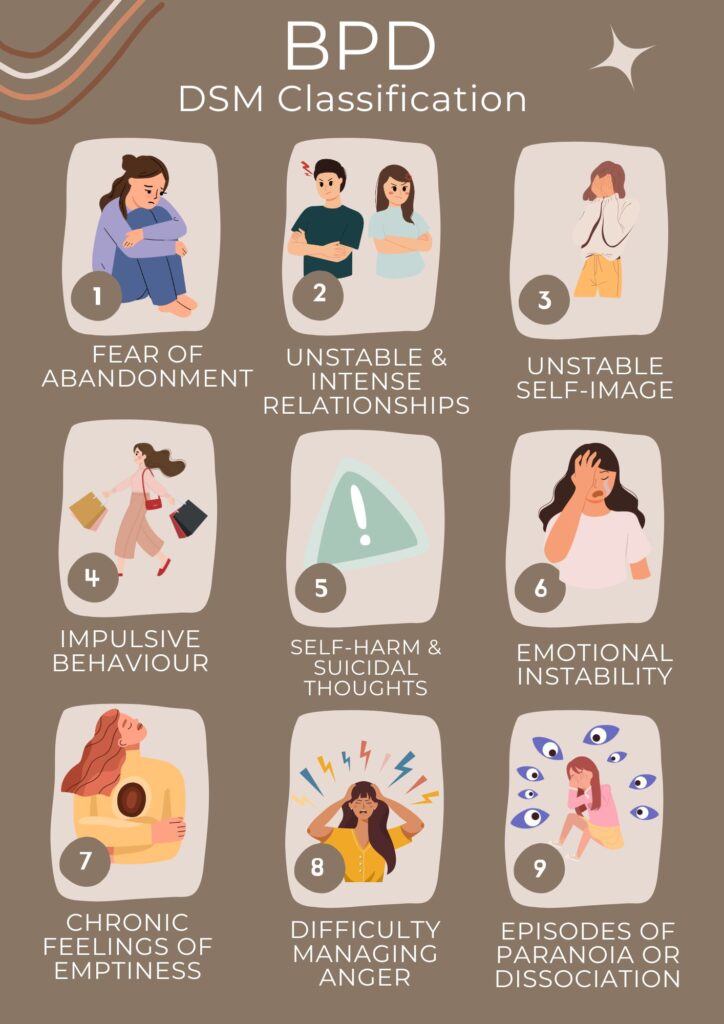
The DSM Classification
BPD is a personality disorder diagnosis, characterised by a consistent pattern of instability. The current definition explains that it manifests as an unstable sense of self-image, having difficulties in interpersonal-relationships, impulsivity or risky behaviour and difficulties managing emotions. The Diagnostic and Statistical Manual of mental disorders (DSM-V) has a classification of nine symptoms. To receive a diagnosis for BPD, five out of nine symptoms must be present in an individual causing significant distress and impairment of functioning. There are as follows (American Psychiatric Association, 2022):
- Fear of abandonment: Experiencing deep-seated fears of being abandoned or rejected which may cause intense emotional distress. Those with BPD may go out of their way to ensure they do not experience these emotions, even when abandonment isn’t imminent.
- Unstable & Intense relationships: Maintaining stable and healthy relationships may be challenging due to this fear of rejection. Sometimes, they may go from idealising a person to feeling deeply hurt by them.
- Unstable self-image: Feelings of confusion and emptiness can come from a shifting sense of identity. Inner turmoil may be consistent due to difficulties defining themselves through goals, values and identity.
- Impulsive behaviour: As a way to cope with difficult emotions, relief may be sought from impulsive or risky behaviour. This may include reckless spending of money, substance abuse, dangerous driving and risky sexual behaviour etc.
- Self-harm and suicidal thoughts: As above, dealing with difficult emotions may also lead to self-harming behaviour and thoughts of suicide. This is usually to manage emotions rather than a desire to end their life.
- Emotional instability: Those with BPD experience emotions more intensely than others, causing rapid shifts in mood and heightened sensitivity to criticism.
- Chronic feelings of emptiness: Despite having a successful life, there may still be struggles with a profound sense of emptiness or loneliness. This can be difficult to manage due to persistence.
- Difficulty managing anger: regulating emotions, particularly anger can be challenging leading to outbursts and conflicts in relationships.
- Episodes of paranoia or dissociation: In times of intense stress, those with BPD can experience episodes of paranoia or dissociation from reality, which can be very distressing.
It is also important to mention that the presentation of BPD varies amongst individuals, not everyone will experience these symptoms in the same way. There are even 4 recognised subtypes of BPD.
What does BPD Stigma Look Like?
I consider myself fortunate to have had a positive experience with my therapist. From the outset, we developed a strong rapport, and I felt safe in her care due to her deep understanding of Borderline Personality Disorder (BPD). However, this is not a universal experience for all individuals seeking therapy. In my time working at a mental health facility, I frequently encountered colleagues who expressed a reluctance to work with clients diagnosed with BPD. Common descriptors used were “attention-seeking” and “manipulative,” reflecting widespread misconceptions. One striking example was a procedural change implemented for one particular client, where staff were instructed to only interact with her in pairs, never individually. This approach seemed to reflect not an effort to understand the client’s needs but rather a reaction based on fear and frustration.
In hindsight, I recognize that feelings of discomfort or hostility often arise from a lack of understanding. Despite working in the mental health field for a decade and attending numerous training sessions on conditions ranging from schizophrenia to hoarding behaviours and substance misuse, I never once encountered formal training on personality disorders, including BPD. A cursory search reveals the existence of such courses, raising questions about why this training was never made available. If stigma within the mental health profession is to be addressed, it is imperative that staff receive appropriate education and training on personality disorders to foster greater understanding and empathy.
Theodore Millon’s 4 Recognised Subtypes of BPD
Theodore Millon was widely respected for his expertise in personality disorders, and his theories on borderline personality disorder have provided mental health professionals with valuable insights and tools to better treat patients. There is no scientific consensus about BPD subtypes but Millon’s classification (Millon,1996) is widely recognised amongst the BPD community, These are:
Discouraged (Quiet) BPD
The key trait here is fear of abandonment leading to extreme actions to avoid abandonment. This may appear in someone as being a perfectionist, high functioning and very successful. However they may struggle to feel connected to others, struggle in group social settings and feel very lonely and isolated. They may engage in self-harm and suicidal behaviour.
Impulsive BPD
This includes impulsive behaviour that can be self-destructive or dangerous. They may appear charismatic, full of energy, engaging to be around and flirtatious. At times they will be detached and elusive.
Petulant BPD
This type presents with unpredictable emotions, they may seem angry, sad or elated at quick intervals. They often feel unlovable leading to controlling behaviour within relationships. Due to feeling out of control, relationships can feel dissatisfying. Addictive behaviour and substances may be used to avoid feelings of emptiness.
Self-Destructive BPD
The self-destructive type will likely engage in various dangerous activities. They are the true self-sabotagers, making risky decisions and acting on impulse destroying any self-progress. They may engage in self-harming behaviour, substance abuse, and seek out adrenaline seeking activities.
Stigma Depends on Traits
As mentioned above, people with BPD will not present in the same way. Public stigma towards people with BPD can differ depending on how their symptoms show up. Since BPD symptoms can vary widely, and to be diagnosed with BPD according to the DSM-5, a person must meet 5 or more of the 9 criteria, which can result in 126 different combinations.
These symptoms may even change over time. From personal experience, I can say that I have been all of these at some time in my life. As a teenager I was often the impulsive type, engaging in risky behaviour. I have always identified with the discouraged type, high functioning, perfectionist who is a bit of a loner! There are times of the month I may be the self-destructive type to some degree. We cannot assume that all people with BPD will display the same behaviour and symptoms, nor that they will be like this forever. Even without the right therapeutic treatments, symptoms of BPD often reduce with age (Biskin R. S, 2015).
Brown (2024) used a model with three subtypes to explore public stigma towards different groups of people with BPD. The first group, labelled “emotional,” included those with intense emotions, impulsivity, and histrionic traits. The second group had low anxiety but showed impulsivity, anger, and high antisocial personality traits. The third group, called “inhibited,” were the least impulsive, less expressive with their emotions, and had avoidant personality traits. Brown found that the public showed the most stigma towards the emotional group, often reacting with anger, fear, and a reluctance to help or interact with them. This suggested that people view this group as more aggressive compared to the other subtypes, which tend to exhibit more inward-focused behaviours like isolation and substance misuse. Unfortunately, this means that individuals with BPD may face more stigma and less support depending on their specific symptoms.
Stigma and BPD: Where does it come from?
As above, the presentation of some symptoms of BPD may be the leading cause of the stigma; suicidal ideation, self-harm and extreme avoidance of abandonment can often be seen by the wider population as manipulative, intentional and attention seeking. Historically, medical professionals even deemed BPD as untreatable. There is a lack of understanding that this behaviour stems from emotional dysregulation and extreme stress which further fuels this perception.
Media portrayals of BPD that I have encountered have often been distressing and difficult to watch. One example that stands out is the depiction of Tony Soprano’s mother in The Sopranos. Tony’s therapist speculates that his mother has BPD due to her manipulative, aggressive, and narcissistic traits; however, I personally did not observe sufficient symptoms to justify a BPD diagnosis. This speculation was mentioned in only one episode, after which the show primarily referred to her as a narcissist, leaving me uncertain about the accuracy and intent behind the terminology used in the writing. It seemed as though the diagnosis was applied without careful consideration.
Another example is Rebecca Bunch from Crazy Ex-Girlfriend. While this series made some effort to delve deeper into empathizing with and understanding someone with BPD, the portrayal was highly exaggerated, and the show’s title itself is problematic, reinforcing stereotypical archetypes.
More recently, I found the media’s obsession with the Amber Heard and Johnny Depp case particularly troubling. Speculation that Amber Heard has BPD was used against her to suggest that she was deceitful and abusive, further perpetuating harmful stereotypes.
In my personal experience, I am frequently dismissed by clinicians when I attempt to discuss physical and mental health conditions. My psychiatrist has been condescending regarding my progress in therapy, expressing surprise at my level of knowledge and understanding of the condition. Additionally, I have had friends who have distanced themselves from me, despite our having been close for ten years prior to my diagnosis. As a result, it is not something I typically disclose when getting to know new people.
This stigma negatively impacts on overall wellbeing, personal and professional relationships, connection with community, accessing healthcare insurance and likelihood to seek help. Despite these implications and the prevalence of this disorder, research and support into BPD is significantly underfunded. It took me 1.5 years of continuously pleading with my Psychiatrist to put me on the Dialectical Behavioural Therapy programme, I assume because I am “high-functioning”.
Overcoming Stigma for BPD
Plenty of people with BPD despise the term borderline, as many dislike emotionally unstable. It is understandable as both make the diagnosis sound confusing and “borderline” is even being misused as a slur. First termed in the 1930’s by the Psychoanalyst Adolph Stern, he noticed some of his patients had the neurotic symptoms of anxiety and depression but they couldn’t be treated with Freudian analysis methods of the time. This led to psychiatrists placing these individuals on a psychotic spectrum, on the borderline between psychosis and neurosis.
Even though we no longer use those terms or methods of analysis, the naming of BPD is still a topic of discussion. Thankfully, many experts now see the term as outdated and not very precise. Over time, the way we think about BPD and other personality disorders might change, since calling something a “personality disorder” suggests that a person’s personality is fundamentally flawed. In reality, it’s more about what a person struggles with rather than their personality being the issue. Some therapists have even proposed renaming BPD to something more accurate and less stigmatising, like Emotion Dysregulation Disorder or Complex PTSD. We may see these changes in the next DSM.
While renaming the disorder would represent progress, it alone would not suffice to change the perceptions held by the public and clinicians regarding individuals with BPD. In recent years, an increasing number of public figures have openly discussed their own diagnoses, which has been a positive step for public perceptions. For example, comedian Pete Davidson has frequently spoken about his struggles with BPD, sharing how the loss of his father in the 9/11 attacks when he was just seven years old contributed to his fear of abandonment, as explored in therapy. Similarly, the late Amy Winehouse publicly battled addiction, depression, self-harm, and impulsive behaviour, leading some doctors to speculate that she may have had BPD following her death in 2011. Additionally, discussions on social media are helping to inform the public about the realities of living with BPD.
Highlighting Positive Traits
It is equally important to highlight the positive traits often associated with individuals who have BPD. Due to the intensity of our emotions, we tend to be exceptionally loving, caring, and empathetic. We are also frequently characterised by creativity, humour, and charisma. Moreover, we tend to be resilient, often recovering from physical and emotional pain more quickly than others. With the acquisition of skills to better manage our emotions, we often develop profound insight, gaining a deep understanding of our thoughts, emotions, and actions.
I will continue to advocate against stereotypes and misconceptions whenever they arise. Stigma often stems from a lack of knowledge and understanding, making it essential to address and correct these misunderstandings when encountered. It is important to politely challenge stereotypes by providing accurate information. Ultimately, a diagnosis does not define a person; just as someone with a broken finger is not referred to as a “broken finger person,” I am a person living with BPD, with one of the 126 combinations of traits, a colourful past and a promising future, not simply a “Borderline.”
Sources
American Psychiatric Association. (2022). Diagnostic and statistical manual of mental disorders (5th ed., text rev.). https://doi.org/10.1176/appi.books.9780890425787
Biskin R. S. (2015). The Lifetime Course of Borderline Personality Disorder. Canadian journal of psychiatry. Revue canadienne de psychiatrie, 60(7), 303–308. https://doi.org/10.1177/070674371506000702
Brown, S. A. (2024). Borderline Personality Disorder Subtypes and Public Stigma. Psychiatry Research Communications, 100176.
Furnham A., Lee V., Kolzeev V. (2015). Mental health literacy and borderline personality disorder (BPD): What do the public “make” of those with BPD? Social Psychiatry and Psychiatric Epidemiology, 50(2), 2. 10.1007/s00127-014-0936-7
Markham, D., & Trower, P. (2003). The effects of the psychiatric label ‘borderline personality disorder’ on nursing staff’s perceptions and causal attributions for challenging behaviours. The British journal of clinical psychology, 42(Pt 3), 243–256. https://doi.org/10.1348/01446650360703366
Millon, T. (1996). Disorders of personality: DSM-IV and beyond.